Urinary And Prostate Disorders
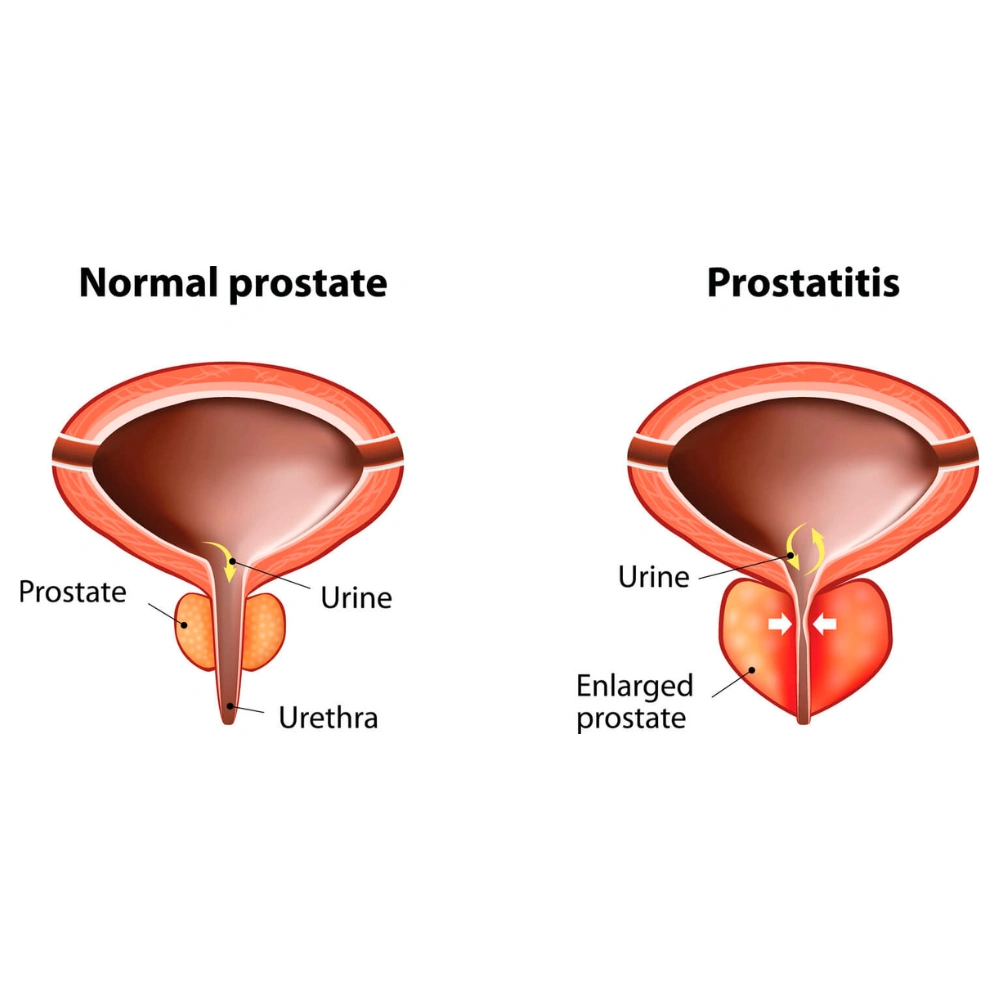
Prostate health extends beyond the gland itself, intricately tied to urinary function. Recognizing the signs is pivotal—symptoms like frequent nighttime urination, urgency, or a weakened stream can signify underlying issues. Regular screenings, including PSA tests, aid in the early detection of prostate cancer. Benign Prostatic Hyperplasia (BPH) assessments involve uroflowmetry, providing insights into urinary patterns. Low Urinary Tract Symptoms (LUTS) demand attention, as they encompass various manifestations affecting daily life. From hesitancy to an abnormal urethral opening, each symptom requires a tailored approach for accurate diagnosis and proactive management, ensuring optimal prostate and urinary health.
Prostate problems often manifest with urinary symptoms, including frequent nighttime urination, increased frequency during the day, sudden and strong urinary urgency, slow initiation of the urine stream, post-void dribbling, a feeling of incomplete bladder emptying, diminished force in the urine flow, and a persistent sensation of needing to urinate shortly after completing the act. These symptoms can be indicative of various prostate conditions and should prompt individuals to seek medical evaluation for proper diagnosis and management.
Screening involves testing to detect cancer in individuals before they exhibit symptoms. In cases where prostate cancer is suspected due to screening results or symptoms, further tests are essential for confirmation. Prostate-specific antigen (PSA) is a protein produced by both normal and cancerous cells in the prostate gland, predominantly found in semen but also present in small amounts in the blood. The PSA blood test is a screening tool used to assess for prostate cancer in men who do not display symptoms, aiding in the early detection and management of the disease.
The doctor conducts a rectal examination to assess the prostate, and you provide a urine sample into a container connected to a machine. This machine, known as uroflowmetry, measures the strength and volume of your urine flow. The results help determine the pattern of urination, and they are compared to age-related norms to assess if it falls within the normal range. Additionally, a postvoid residual volume test is performed to determine if your bladder empties fully. This test may involve an ultrasound imaging exam to evaluate the remaining urine volume after voiding. These assessments contribute to a comprehensive evaluation of urinary function and potential prostate issues.
Low Urinary Tract Symptoms (LUTS) encompass a range of manifestations that can significantly impact an individual’s urinary function and overall well-being. Increased daytime and nighttime frequency, where there’s a sensation of being unable to fully empty the bladder or an accelerated filling of the bladder, often characterizes LUTS. Urgency, marked by a sudden, compelling need to urinate, is another common symptom. Individuals experiencing LUTS may also notice an increase in the volume of urine passed, along with a heightened frequency of urination, particularly during nighttime. The presence of burning sensations and pain during urination adds to the complexity of these symptoms, creating a challenging and uncomfortable urinary experience. These manifestations may arise from various underlying conditions, and seeking medical attention is crucial for an accurate diagnosis and tailored management plan to address the specific causes of LUTS.
A weak or intermittent urine stream, often accompanied by difficulties initiating or sustaining the flow, can indicate various underlying health issues. One common cause is an enlarged prostate in men, which can obstruct the urinary passage. In women, pelvic organ prolapse may contribute to similar symptoms. Other potential factors include urinary tract infections, neurological disorders affecting bladder control, or muscle weakness in the pelvic region. Conditions like interstitial cystitis and urethral stricture can also lead to a compromised urine stream. Additionally, medications, dehydration, or psychological factors may influence urinary function. Seeking medical advice is crucial to identify the specific cause and determine an appropriate course of action for addressing the weak or irregular urine stream. Early intervention can help manage the underlying condition and improve overall urinary health.
Straining during urination, or difficulty initiating the process of emptying the bladder, can be indicative of various underlying conditions. One common cause is an enlarged prostate in men, which can create an obstruction in the urethra, leading to difficulty in initiating and completing urination. In women, pelvic organ prolapse may contribute to straining. Other potential causes include urinary tract infections, bladder stones, or neurological issues affecting the coordination of bladder muscles. Straining can also result from weak pelvic floor muscles. It is essential to consult with a healthcare professional to determine the specific cause of straining during urination and to receive appropriate diagnosis and treatment for optimal urinary health.
Hesitancy in initiating urine flow and experiencing an intermittent stream can be indicative of various underlying medical conditions affecting the urinary system. One common cause is an enlarged prostate, especially in older men, which can obstruct the urethra and impede the smooth flow of urine. Conditions like urinary tract infections (UTIs) or prostate inflammation may also contribute to hesitancy and irregular urine stream. Neurological issues, such as nerve damage or multiple sclerosis, can affect the coordination of bladder muscles, leading to difficulties in initiating and maintaining a steady urine flow. In some cases, medications or anxiety-related factors may contribute to these symptoms. Prompt consultation with a healthcare professional is essential for a thorough evaluation, including a physical examination and possibly diagnostic tests, to determine the underlying cause and devise an appropriate treatment plan to alleviate the hesitancy and improve the flow of urine.
The prostate, an essential part of the male reproductive system, undergoes changes with age. These changes can lead to two main conditions: benign prostate enlargement (BPH) and prostate cancer. BPH is a non-cancerous growth that can cause urinary symptoms, while prostate cancer involves malignant cell growth. Regular check-ups, including tests like PSA blood tests and digital rectal exams, are crucial for early detection and effective management. Monitoring prostate health is especially important for aging individuals, as prompt intervention can make a significant difference in addressing both benign and malignant prostate issues.
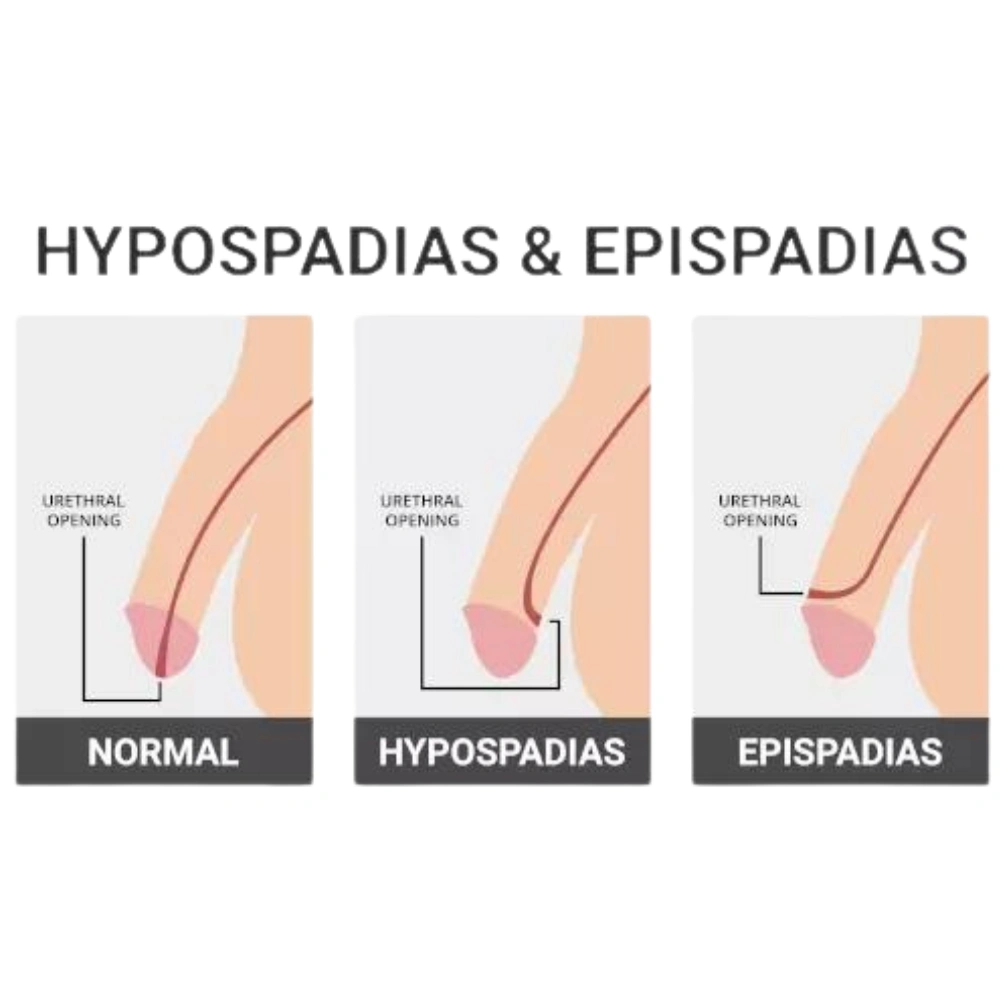
When the opening of the urethra is in an abnormal position due to a congenital condition, it can affect both urination and ejaculation. This misplacement can lead to issues like difficulty emptying the bladder completely and an increased risk of urinary tract infections. Additionally, it may impact sexual functions by causing challenges in achieving or maintaining an erection and affecting the force and trajectory of ejaculation. If someone experiences symptoms related to this issue, it’s important to consult a healthcare professional for evaluation and potential corrective measures.
Urethral stricture refers to the condition where the urethra, the tube responsible for carrying urine from the bladder out of the body, becomes narrowed. This narrowing can occur due to various reasons, including infections, certain medical procedures, or for no apparent reason (idiopathic). Infections, such as those from sexually transmitted diseases or urinary tract infections, can lead to inflammation and scarring, contributing to the constriction of the urethra. Medical procedures, like catheterization or urethral surgeries, may inadvertently cause narrowing (iatrogenic).
Urethral strictures can have significant implications for urinary and ejaculatory functions. Individuals with this condition may experience difficulty in urination and ejaculation. If left untreated, strictures may obstruct the normal flow of urine, potentially leading to complications and affecting kidney function over time.
Fortunately, there are effective treatment options available. Endoscopic procedures or surgical interventions can help alleviate the stricture, allowing for the restoration of normal urinary and ejaculatory functions. It is crucial for individuals experiencing symptoms or diagnosed with urethral stricture to seek timely medical attention to address the condition and prevent potential complications.
Urethral injuries resulting from trauma or accidents can lead to the rupture and dissociation of the urethra, where the tube responsible for carrying urine from the bladder is disrupted. Surgical intervention can successfully realign and repair the damaged urethra in these cases. This surgical alignment is crucial for restoring normal urinary function and preventing complications associated with untreated urethral injuries. Swift medical attention and appropriate surgical procedures play a pivotal role in achieving successful outcomes and minimizing long-term consequences.
Health Tips & Info
Prostate problems often manifest with urinary symptoms, including frequent nighttime urination, increased frequency during the day, sudden and strong urinary urgency, slow initiation of the urine stream, post-void dribbling, a feeling of incomplete bladder emptying, diminished force in the urine flow, and a persistent sensation of needing to urinate shortly after completing the act.
Screening involves testing to detect cancer in individuals before they exhibit symptoms. In cases where prostate cancer is suspected due to screening results or symptoms, further tests are essential for confirmation. Prostate-specific antigen (PSA) is a protein produced by both normal and cancerous cells in the prostate gland, predominantly found in semen but also present in small amounts in the blood. The PSA blood test is a screening tool used to assess for prostate cancer in men who do not display symptoms, aiding in the early detection and management of the disease.
The doctor conducts a rectal examination to assess the prostate, and you provide a urine sample into a container connected to a machine. This machine, known as uroflowmetry, measures the strength and volume of your urine flow. The results help determine the pattern of urination, and they are compared to age-related norms to assess if it falls within the normal range. Additionally, a postvoid residual volume test is performed to determine if your bladder empties fully. This test may involve an ultrasound imaging exam to evaluate the remaining urine volume after voiding.
The doctor conducts a rectal examination to assess the prostate, and you provide a urine sample into a container connected to a machine. This machine, known as uroflowmetry, measures the strength and volume of your urine flow. The results help determine the pattern of urination, and they are compared to age-related norms to assess if it falls within the normal range. Additionally, a postvoid residual volume test is performed to determine if your bladder empties fully. This test may involve an ultrasound imaging exam to evaluate the remaining urine volume after voiding.
A weak or intermittent urine stream can indicate various underlying health issues. One common cause is an enlarged prostate in men, which can obstruct the urinary passage. In women, pelvic organ prolapse may contribute to similar symptoms. Other potential factors include urinary tract infections, neurological disorders affecting bladder control, or muscle weakness in the pelvic region. Conditions like interstitial cystitis and urethral stricture can also lead to a compromised urine stream.

